Health Workers Are Optimistic About Industry's Future as COVID-19 Wanes
Series Introduction
Since the start of the COVID-19 pandemic, many health care workers have left the industry amid unprecedented stress and trauma. New Morning Consult data from roughly a thousand health care workers shows signs of optimism, but challenges remain as workers contend with staffing shortages, insufficient wages and an ever-increasing political environment.
Read our coverage: Labor Challenges | Abortion Policies
Key Takeaways
58% of health care workers said they are optimistic about the future of the industry, compared with 37% who said they are pessimistic.
Equal shares of health care workers (42%) said they felt either “energized” or “defeated” by work in the past six months.
Roughly 3 in 5 said their facilities are prepared for the end of the emergency declaration.
For our latest global health care data and analysis, sign up for our daily health news briefing.
The COVID-19 pandemic has stretched the U.S. health system to its limits over the past three years, with health care workers — especially front-line staff — forced to struggle through patient surges, workforce shortages and dangerously low supplies of personal protective equipment.
Over this time, many health workers have experienced burnout, stress and trauma, which has forced some to leave the industry.
While the pandemic is not over, despite the end of the U.S. public health emergency in May, nearly 3 in 5 health care workers said they are optimistic about the future of the industry, according to a new Morning Consult survey. Another 3 in 5 said they have mostly been able to handle the stressors of work in the past six months.
“It was a lot of change coming at the health care field very, very quickly,” said Akin Demehin, senior director of quality and patient safety policy at the American Hospital Association. “Now, we're sort of in this new phase where the public health emergency has just ended, the most emergent phase of the pandemic has concluded [and] we have vaccines that we know are incredibly effective at keeping patients out of the hospital.”
He added that the U.S. health system has “been dramatically affected — in some ways traumatized — and in many ways transformed.”
3 in 5 Health Workers Say They Have Been Able to Cope With Work Stress in the Past 6 Months
Atul Grover, executive director of the Association of American Medical College’s Research and Action Institute, said providers are now seeing a lower number of severely ill patients since COVID-19 cases have declined, which has helped alleviate some of the stress on hospital and health workers. He added that early strategies that hospitals and health facilities implemented to keep the virus from spreading closed family members off from patients, putting a lot of emotional responsibility onto the people taking care of them.
“A lot of these things that, as physicians and health care workers, we're used to seeing some of and experiencing some of. But just that barrage of death and illness and acuity, I think was very hard on people,” Grover said.
COVID-19 hospitalizations recently hit a record low, and hospital systems have returned to a more normalized environment. However, the industry still faces pressures that were exacerbated by the pandemic but existed before, such as wage disputes and staff shortages.
Specific demographics at scale: Surveying thousands of consumers around the world every day powers our ability to examine and analyze perceptions and habits of more specific demographics at scale, like those featured here.
Why it matters: Leaders need a better understanding of their audiences when making key decisions. Our comprehensive approach to understanding audience profiles complements the “who” of demographics and the “what” of behavioral data with critical insights and analysis on the “why.”
Health workers still feel stressed and burned out by their jobs three years into the pandemic: 1 in 3 said they have struggled to cope with the stressors of work in the past six months, and respondents were split on whether they felt defeated by the demands of their work or energized in the past six months (42% for each).
Nearly half of those who said they have felt defeated by work have been affected by staff shortages (48%), double the share who said they have not been affected by shortages.
Majority of health workers say their facilities are prepared for the end of the COVID-19 PHE
As the United States transitions out of the COVID-19 PHE, about 3 in 5 health care workers said their facilities are prepared to handle the end of the emergency declaration and have an appropriate amount of PPE for a potential increase of COVID-19 patients, while more than half said they are prepared to handle future surges.
Majority of Health Workers Say Their Facilities Are Prepared to Handle COVID-19 Surges, Have Proper PPE Supply
Half of health care workers said their facilities are prepared to handle surges of multiple illnesses at the same time, such as COVID-19 and RSV and/or influenza, a dynamic that overflowed hospitals last winter even though coronavirus cases were relatively low.
AHA’s Demehin said last winter was unprecedented and put additional strain on providers. He argued that it is important to make pandemic-era flexibilities for telehealth and virtual care permanent to help hospitals, emergency rooms and urgent care clinics remain open for the sickest patients.
“It is going to continue to be a challenge,” Demehin said. “I wish I could tell you that the variants of COVID-19 will remain fixed over time — I'm sure we're going to see an evolution to that. So, as it comes, I know hospitals will be continually adapting.”
Health workers split on the impact of the end of PHE policies
The majority of health workers surveyed said their facility is prepared for the end of the COVID-19 PHE, but that does not mean that the end of the declaration will have no impact on their work. Workers were split as to how much of an effect the end of certain policies will have.
More than half (55%) said the removal of policies that expand Medicare or Medicaid services will have an impact, including 3 in 10 who said it will have a “major” impact, the most of any change surveyed. Meanwhile, about 1 in 3 said there will be no impact to those services, the least of any change surveyed.
Health care workers were more divided on the impact of other coverage- and funding-related COVID-19 policies.
Removal of Policies to Expand Medicaid, Medicare Services Will Have Biggest Impact on Health Workers’ Jobs
With the end of the PHE declaration and low levels of COVID-19 hospitalizations and deaths, the health industry has other challenges on which to now focus. A top priority for most is addressing the workforce shortage that impacts a list of specialties.
“The level of urgency to address workforce issues remains as high as it's been at any point,” Demehin said, “and most certainly in the wake of the COVID-19 pandemic.”
Ricky Zipp previously worked at Morning Consult as a health care analyst on the Industry Intelligence team.
Related content
Health Workers Impacted by Staff Shortages More Likely to Consider Quitting
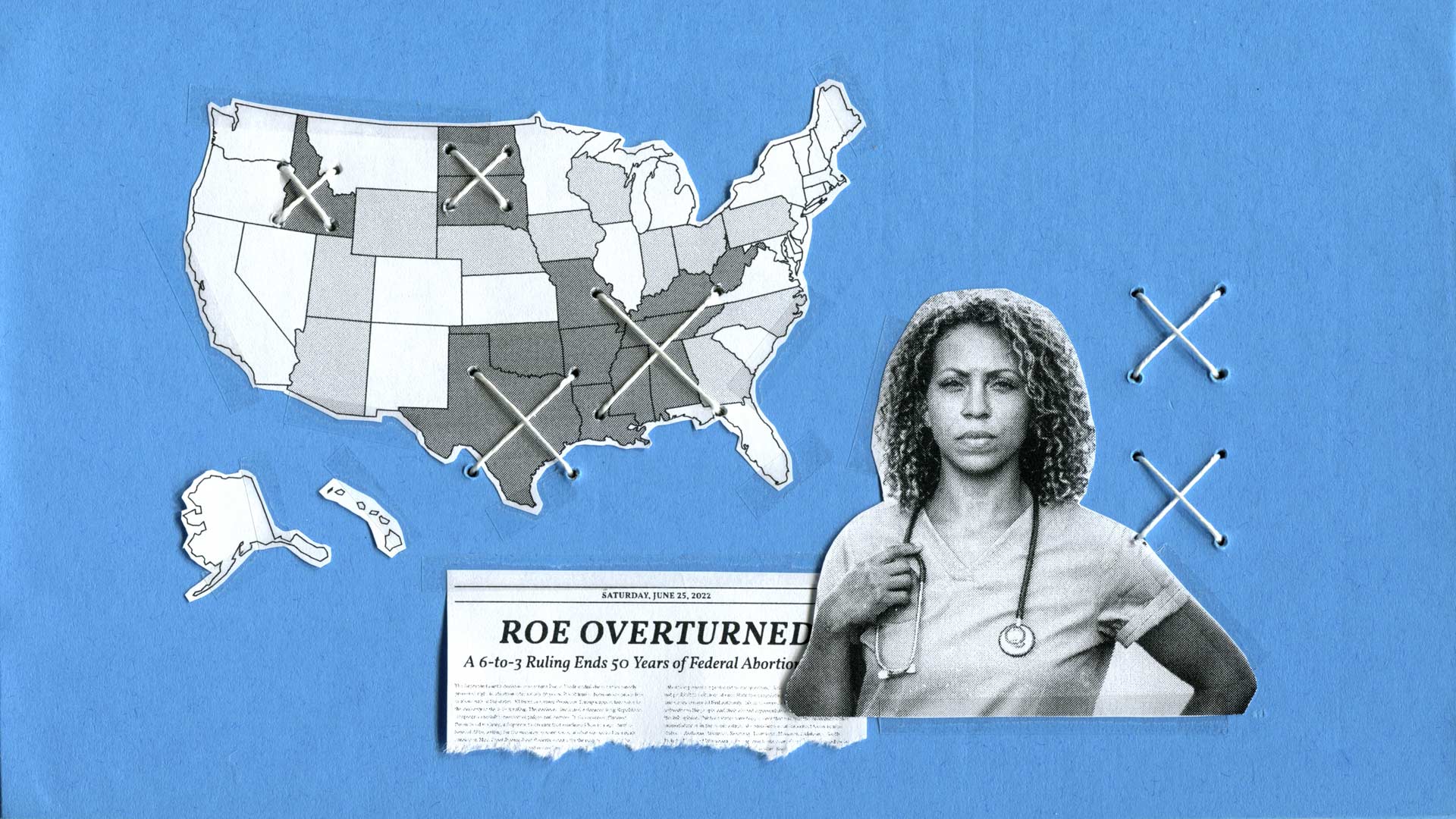
Some Health Workers Are Considering Quitting, Moving Over Abortion Bans