Health Workers Impacted by Staff Shortages More Likely to Consider Quitting
Series Introduction
Since the start of the COVID-19 pandemic, many health care workers have left the industry amid unprecedented stress and trauma. New Morning Consult data from roughly a thousand health care workers shows signs of optimism, but challenges remain as workers contend with staffing shortages, insufficient wages and an ever-increasing political environment.
Read our coverage: Industry’s Future | Abortion Policies
Key Takeaways
2 in 5 health care workers said the national staff shortage has had a “major” impact on their job and facility, while about 1 in 3 said it has had a “minor” impact.
About a quarter of health care workers said shortages have had no impact on their job or place of work.
Workers who have been impacted by shortages were more than twice as likely to say they have considered leaving their job in the past year than workers who have not been impacted by shortages.
For our latest global health care data and analysis, sign up for our daily health news briefing.
The COVID-19 pandemic put a national spotlight on the environmental conditions health care professionals faced even before the crisis, including wage issues and staffing shortages. But the pandemic simultaneously created an emergency situation that took focus away from solving those myriad challenges.
As COVID-19 hospitalizations continue to decline and the United States transitions out of the national and public health emergencies, health care workers and experts are demanding that hospitals and health facilities once again address labor issues — particularly staff shortages — before it is too late.
Nearly 3 in 4 health care workers said the national staff shortage has impacted them and their facilities, including 2 in 5 who said it has had a “major” impact, according to a new Morning Consult survey. Conversely, about 1 in 4 said the national shortage has had no impact.
Deena Kelly Costa, associate professor of nursing and medicine at Yale University’s School of Medicine, said the COVID-19 pandemic “turned up the volume” on understaffing and “made it a lot more visible.”
Multiple industry experts agreed that the issue needs to be prioritized, cautioning that understaffing creates a cyclical effect where shortages lead to burnout, forcing even more people out of the industry, which then creates more shortages at facilities.
2 in 5 Health Workers Say Staffing Shortages Have Had Major Impact on Their Work
Renée Saldaña, press secretary for SEIU-United Healthcare Workers West, said people “were banging pots and pans” to show support for health workers and employers were saying “thank you to our health care heroes” during the early days of the pandemic.
“Now, a lot of these same employers are not providing wage increases that keep up with the cost of living,” she added. “They are still seeing short staffing in their facilities. They have watched many of their co-workers — especially the ones who are at the lower end of the wage scale — they're watching those folks leave in droves.”
Many health workers have considered leaving their job in the past year
Employee shortages have been an issue facing the health care industry for years, impacting physicians, specialists, nurses and other professions. According to a 2021 report from the Association of American Medical Colleges, the United States could see a physician shortage between 37,800 and 124,000 by 2034 depending on the policies implemented to address the problem, including a shortage of up to 48,000 primary care physicians.
The pandemic has also forced some people out of the industry. More than 100,000 registered nurses left the profession in 2021, a “far greater drop than ever observed over the past four decades,” according to an April 2022 Health Affairs article.
Christopher Friese, professor of health management and policy at the University of Michigan’s School of Public Health, said that the issue of nursing shortages affects the safety of both workers and patients.
“I'm increasingly concerned that the window of time to right the ship is narrowing,” Friese said. “I am very concerned that health care executives appear to expect this all to go away magically — and that's a real mistake.”
While COVID-19 hospitalizations have recently dropped and last winter did not see the level of surges as previous years, the new Morning Consult survey shows the toll the industry is still taking on people who work in health care facilities.
Specific demographics at scale: Surveying thousands of consumers around the world every day powers our ability to examine and analyze perceptions and habits of more specific demographics at scale, like those featured here.
Why it matters: Leaders need a better understanding of their audiences when making key decisions. Our comprehensive approach to understanding audience profiles complements the “who” of demographics and the “what” of behavioral data with critical insights and analysis on the “why.”
Among health care workers who have kept their jobs over the past year, 41% have considered leaving during that time frame, compared with 31% who said they considered leaving their employer during the pandemic in a September 2021 survey. About 1 in 5 said they have considered leaving the health care industry altogether, a similar share as the 2021 survey.
The most recent survey also shows the impact shortages can have on health workers: Half of those who have been affected by shortages said they have considered leaving their jobs in the past year, more than double the share who have not been impacted by shortages.
Half of Health Workers Impacted by Staffing Shortages Say They Have Thought About Leaving Their Job in the Past Year
Experts say the industry should focus on retention, not recruitment strategies
Ashley Darcy-Mahoney, a neonatal nurse practitioner and associate professor of nursing at George Washington University, said that understaffing is impacting many health professions but nurses are in a unique position: While other professions have to recruit, educate and train professionals to address shortages, nursing is dealing with vacancies despite the thousands of trained nurses who are not working in the industry.
“We're seeing a substantial vacancy issue,” said Darcy-Mahoney, who estimated a rate of at least 25% in hospitals. “The data suggests that we, again, have enough nurses, but nurses don't want to work in places where they're undervalued, unsupported — where they work in systems that create this high level of burnout and compassion fatigue.”
Costa and Friese, who co-authored a paper published last year in the New England Journal of Medicine, both said that health facilities should focus more on retention strategies rather than recruitment strategies to address nursing shortages — implementing changes like higher wages and even offering on-site child care as approximately 90% of the profession are women.
One solution to address nursing understaffing would be mandatory staff-to-patient ratios, Costa and Friese said.
California and Massachusetts have enacted staff ratio policies, and Sen. Sherrod Brown (D-Ohio) and Rep. Jan Schakowsky (D-Ill.) introduced legislation in March that would implement federal minimum nurse-to-patient ratios. But there has been pushback to the strategy.
In Minnesota, a staff ratio provision was recently stripped out of legislation after it was criticized by the Minnesota Hospital Association and an exemption was granted to the Mayo Clinic. The American Hospital Association, the country’s leading provider industry group, said in a statement to the House Energy and Commerce Health Subcommittee that nursing staffing ratios were restrictive, adding that “staffing ratios are a static and ineffective tool that does not guarantee a safe health care environment or quality level to achieve optimum patient outcomes.”
Friese said that he used to think it was more important to address the environment of work and focus on employment flexibilities rather than staff ratios. However, the lack of change within the industry to solve what most consider a major issue has changed his mind, and it has also led to state and federal legislation.
“We have current staffing plans that are primarily set for economic reasons and efficiency reasons. They're not set from a safety perspective — they very rarely take into account what a nurse believes this patient needs in terms of nursing care,” Friese said. “Hospitals and health systems could implement their own plan tomorrow that would be the minimum floor for safety, and they choose not to do that.”
The staffing shortage is one of several labor issues currently facing the industry. Nurses and other health employees have been in contract disputes or gone on strikes across the country, demanding better wages and other changes to their work environment, with shortages being a priority.
Costa argued that one reason there is pushback when it comes to demands for higher wages and better staffing levels is that professions in hospitals and health fields like nursing are undervalued and face an unbalanced power dynamic that has existed throughout the history of the profession.
“We don't get uncomfortable talking about physician pay for performance, and their relative value units and the amount of money that they bring into the organization,” Costa said. She added that because of sexist or patriarchal power structures in society and the industry, nursing is often seen as a profession that should be done out of the goodness of your heart, which has “led to some of these challenges.”
Despite the ongoing challenges, health care workers, educators and policy experts remain relatively optimistic about the future of nursing and health care.
“They could just walk away from their jobs and go somewhere else, but they don't because they love it,” SEIU-UHW’s Saldaña said. “They want to stay and fight, and they think that now the nation understands how vital every single health care worker is to our system.”
Ricky Zipp previously worked at Morning Consult as a health care analyst on the Industry Intelligence team.
Related content
Health Workers Are Optimistic About Industry's Future as COVID-19 Wanes
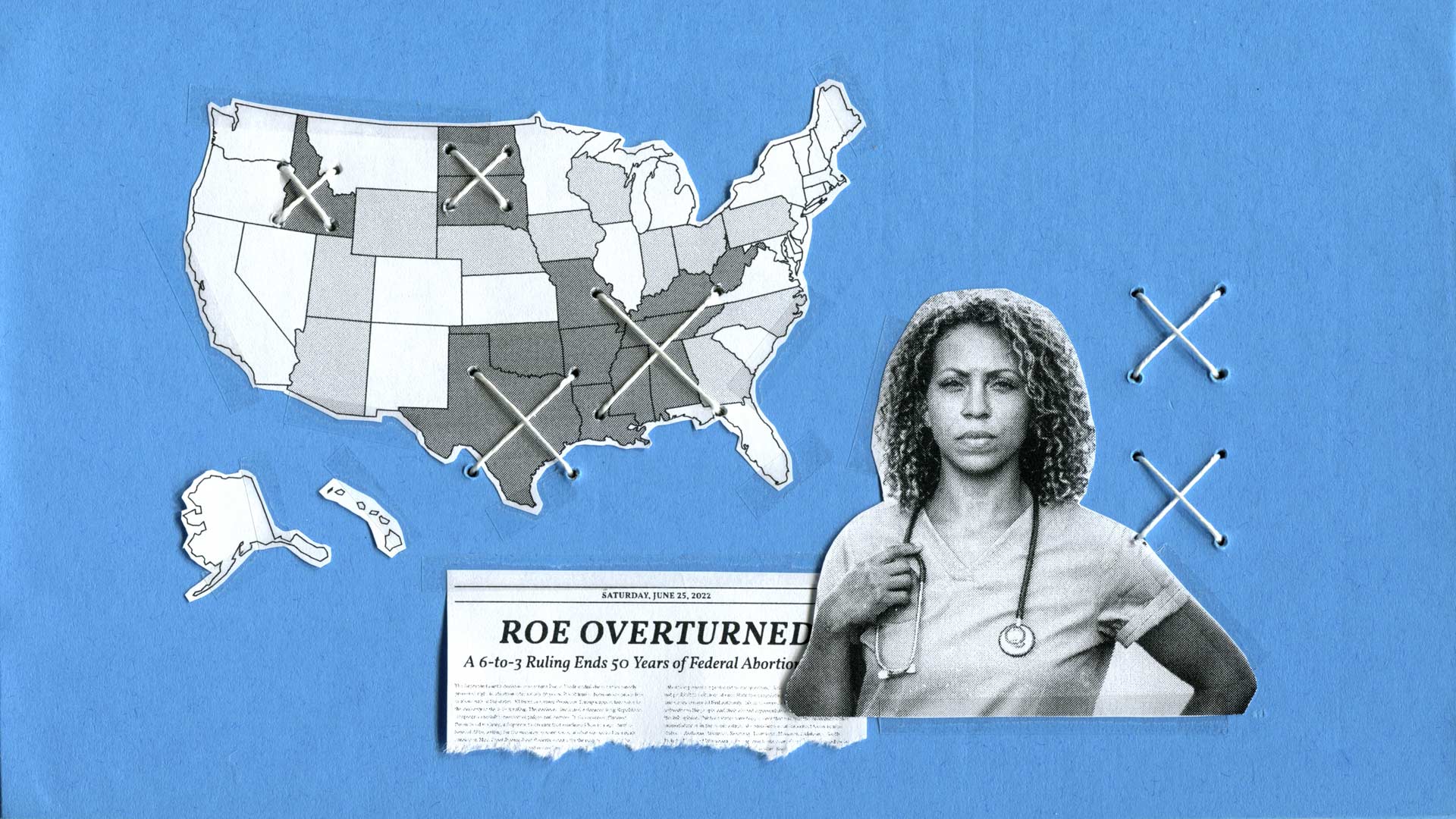
Some Health Workers Are Considering Quitting, Moving Over Abortion Bans